Marie-Louise ConnollyHealth correspondent, BBC News NI
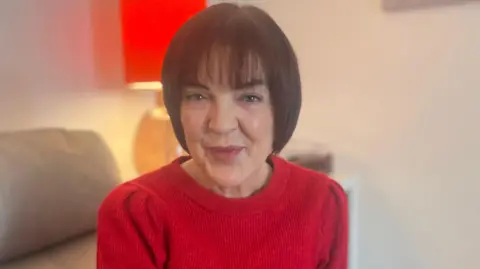 BBC
BBCJennifer Dummigan’s cancer journey was different to that of most people in Northern Ireland.
In December 2023, she noticed symptoms – a chest tickle and discomfort while eating. A GP visit in March led to a diagnosis of oesophageal cancer in May and treatment in July.
From first contact with a doctor to a treatment plan, five months.
But data shows that it is a different story for many people in Northern Ireland, who face a long time on waiting lists, with a major charity, Cancer Research UK, warning emergency measures must be introduced to protect patient safety.
Northern Ireland’s devolved Department of Health (DoH) said cancer waiting times “are not acceptable and remain a priority” and that it is working with health trusts “to address the underlying issues”.
For Dummigan, her recovery was all down to not having to wait for a diagnosis or treatment.
Dummigan, who is 54 and lives in Craigavon, said she had enormous sympathy for people who were on waiting lists as every day, week and month can make a difference to a person’s prognosis.
“My prognosis was so good because I was seen so quickly,” she told BBC News NI.
She said recent scans indicated that she was “cancer free” at the minute, and she “definitely” attributes that “to the speed of treatment and the teams at the cancer centre”.
“The hospital team was superb,” she said. “I was diagnosed with stage two cancer and had chemotherapy for five weeks.
“An oesophagectomy was carried out in October, but recovery has been slow with some minor setbacks.”
An oesophagectomy is major surgery to remove part or all of the oesophagus (food pipe) and involves connecting the remaining oesophagus to the stomach (or sometimes intestine) to restore digestion.
‘Treatment should be equal’
Dummigan said that alongside the physical trauma of coping with cancer, the mental angst could be just as traumatic.
“One of my friends was waiting on a list for six months whereas I was six weeks – she was almost cross – even angry – with me because I was seen so quickly,” she added.
Dummigan, who is a diabetes prevention health coach in the Southern Health Trust, said access to timely treatment should not be a postcode or cancer type lottery.
“It should be down to the health service, and everyone should have equal access to timely services no matter what type of cancer,” she said.
Cancer services ‘in crisis’
 Cancer Research UK
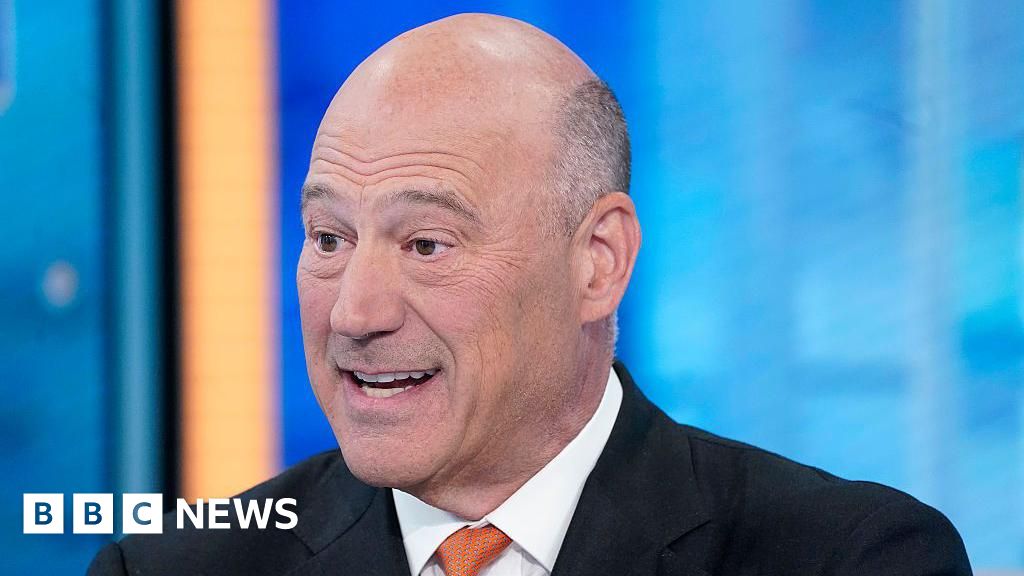
Cancer Research UKSpeaking to BBC News NI, Cancer Research UK’s director of evidence Naser Turabi said it was “absolutely critical” that those patients with the highest critical need should be prioritised, adding that this would require a system-wide approach.
He said cancer delays significantly affect outcomes, increasing mortality risk, worsening prognosis and reducing survival chances.
Turabi said studies show even a one-month delay raises death risk by 6-10% for common cancers, impacting quality of life and increasing psychological stress.
He has urged the Northern Ireland Executive to develop an emergency stabilisation plan.
“We need to see immediate action to protect patient safety by reducing the backlog of people still waiting for diagnosis and treatment,” Turabi said in a statement.
Northern Ireland’s missed cancer targets
The number of patients referred with suspected cancer and the number requiring treatment is increasing in every UK nation.
However, the rise has been predicted and is consistent across all the nations, yet it has not led to such steep declines in waiting‑time performance as seen in Northern Ireland, according to a new report from Cancer Research UK.
In the past five years, the charity said about 15,400 patients in Northern Ireland started their treatment later than the 62-day target following a red flag referral.
The report reveals that the number of people in Northern Ireland starting treatment per month – after red flag referral – has more than doubled between 2008 and 2025.
Current statistics predict that waiting times will get worse and over the next five years – as about 20,000 people will not start treatment on time.
 Getty Images
Getty ImagesLatest official statistics, for the quarter ending September 2025, show performance across all key targets have not been met:
- 31-day target (decision to treat to treatment):
Performance: 88.0% of patients started treatment within 31 days that’s up slightly from the previous quarter
Target: At least 98%
- 62-day target (urgent GP referral to treatment):
Performance: 30.1% of patients started treatment within 62 days.
Target: At least 95%
Trend: A decrease from 32.5% in the previous quarter
- 14-day target (urgent breast cancer referral to specialist):
Performance: 6.8% of patients were seen within 14 days
NI cancer times worst in UK
Cancer times in Northern Ireland are by far the worst in the UK.
As part of its new report, Cancer Research UK has set out steps on how Northern Ireland’s health and social care system can act to better protect patients.
They include:
- Prioritising patients who are most at risk
- Scrutinising the number of people who need tests and treatment and acting quickly on pressure points
- Tracking every patient’s cancer journey so it is clear and moving them along each step where possible
- Setting realistic improvement goals for each trust and speciality
DoH working to address ‘underlying issues’
In a statement, the DoH said it welcomed the charity’s report and it is working with “trusts to address the underlying issues by strengthening cancer pathways, improving capacity across diagnostics and treatment, and continued tracking of patients through their cancer journey”.
“Investment through the Elective Care Framework and the NI Cancer Strategy is supporting the expansion of endoscopy and CT/MRI services and improvements across a number of tumour sites,” a spokesperson added.
“These actions, delivered in partnership with trusts and system partners, will help to deliver sustainable and equitable cancer services for patients and families across Northern Ireland.”