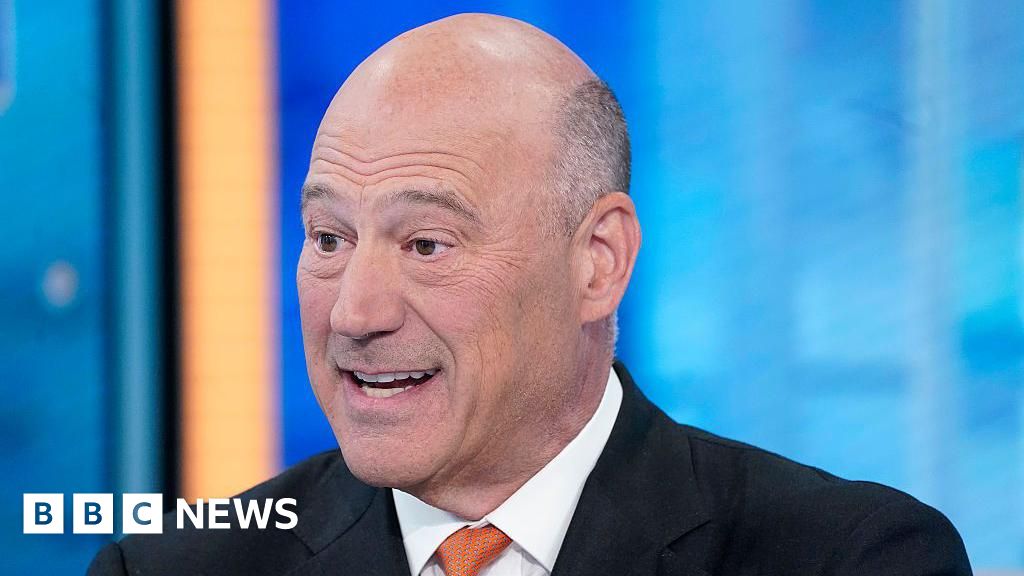
PA Media
PA MediaEmergency departments (EDs) in Northern Ireland are “not in a good position” to deal with continuing winter pressures, Health Minister Mike Nesbitt has said.
Nesbitt said he had spoken to a number of ED staff over the last week, who told him “either this is as bad as it has ever been, or it is actually worse than it has ever been”.
It comes after figures from New Year’s Eve showed that more than half of the 892 people who attended EDs had to endure a wait of more than 12 hours.
On Thursday, Dr Clodagh Corrigan, deputy chair of the British Medical Association in Northern Ireland, said the impact of winter pressures has filled staff with fear for the weeks ahead.
Nesbitt said he also feared for the coming weeks “because one of the things that has tipped us into this incredibly difficult position is the flu”.
“Modelling from the past would suggest that’s not going to peak for another one to two weeks, so we are not in a good position at all,” he told BBC News NI’s Good Morning Ulster programme.
 Getty Images
Getty ImagesNesbitt said that he was also concerned about staff morale.
“They didn’t sign up to deliver a service like this; they wanted something better.”
He added that patients expected “an appropriate level of privacy”, which “does not always happen because of the nature of the demand at the moment in EDs”.
Almost 400 people were waiting for a hospital bed in Northern Ireland last week, with flu and respiratory infections affecting many people.
Winter Preparedness Plan
The department’s Winter Preparedness Plan, published in November, is “mitigating” the challenges, Nesbitt said.
However, he added: “We are focusing quite rightly on EDs, but that is not the problem; that is just where the problem manifests itself.
“It’s a system-wide problem, and in terms of hospitals, it’s about the flow, getting people in the front door, and then getting them out the back door after they get the medical process they need.”
Nesbitt said that in late February or early March he plans to bring all stakeholders together to “start with a blank page and see what we can do to make sure this doesn’t happen again when we get to the winter of 2025”.
Pharmacy impact
Gerard Greene, head of Community Pharmacy NI, said pharmacies were also “extremely busy at the minute”.
“We’re hearing people describe it as relentless,” he said.
“We’re seeing a lot of pressure, a lot of requests coming from patients into pharmacies.”
Mr Greene said people were picking up on public messaging from the Department of Health encouraging them to use the appropriate part of the health service for symptoms, for example, going to pharmacies initially to avoid putting pressure on GPs, out of hours and EDs.
 Brian Thompson
Brian Thompson“We are seeing a lot more people presenting at pharmacies looking for advice and treatment,” he said.
“It’s about looking after patients. We’re trying to help and play our part in managing the demand and taking the pressure off GPs, out-of-hours, etc.
“It’s about using the resource as best as possible. Community pharmacy, since the pandemic, has stepped forward in terms of what we can do.”
He said pharmacies now offer a much wider range of services, with the Pharmacy First service enabling a range of conditions to be treated in pharmacies.
“More significant” conditions like UTIs can also be treated, he said, and pharmacies are offering pilot shingles services and vaccinations.